Whitehouse Opening Statement at Hearing on Alleviating Administrative Burdens in Health Care
“There is a lot of non-clinical work incidental to the actual delivery of care. … [It’s] a dizzying web of administrative functions costing over half a trillion dollars per year”
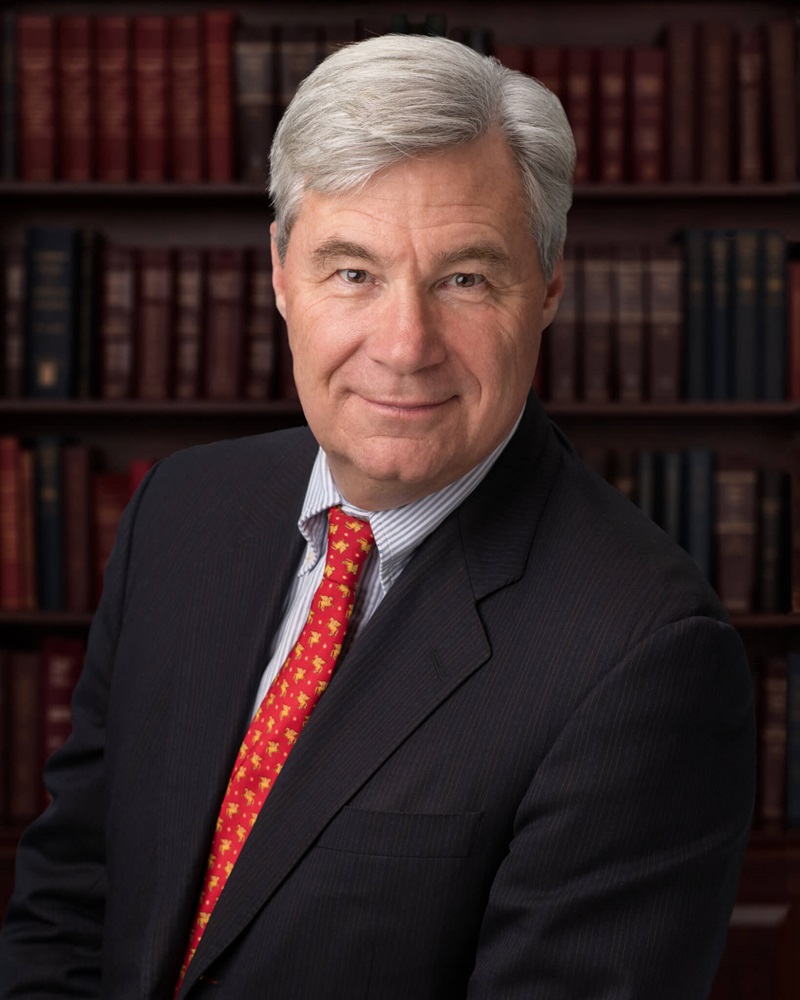
Washington, D.C.— U.S. Senator Sheldon Whitehouse (D-RI), Chairman of the U.S. Senate Budget Committee, delivered the following opening statement at today’s hearing, titled “Reducing Paperwork, Cutting Costs: Alleviating Administrative Burdens in Health Care.”
Chairman Whitehouse’s remarks, as prepared for delivery:
Ranking Member Grassley and members of the committee, today’s hearing will examine administrative cost in health care, how it harms patients and providers, and how much it increases federal health care costs.
There is a lot of non-clinical work incidental to the actual delivery of care, mostly related to getting paid. Our hearing last October spotlighted a dizzying web of administrative functions costing over a half a trillion dollars per year. Of course, this is not just a matter of dollars and cents – lives are at stake.
One of my constituents, Deb from Cumberland, faced cruel insurance hurdles in the wake of a brain tumor diagnosis. She said, “If fighting this disease wasn’t enough to deal with, I and others are constantly fighting with insurance companies who are trying to deny every treatment path. For some reason, they feel that they know what’s better for us than the medical community.”
For as long as I have served in the Senate, we have been discussing how to untangle this web of administrative burdens. As we worked on the Affordable Care Act, I highlighted how the broken economics of the health care system drove these administrative costs. The ACA made some strides in alleviating administrative burdens in the financial transaction ecosystem in health care. Specifically, we set forth standard operating rules for electronic funds transfers and standardization of certain claims forms, producing less friction in the exchange of information between providers and insurers, facilitating faster care delivery for patients.
But there is more to do. Billing and insurance-related costs still total nearly $200 billion a year. The lack of standardization has been one major pain point. Different insurers apply different processes and rules to different providers, creating a web of confusion, driving up costs and making doctors sometimes spend more time on administration than on actual care. The inconsistent paperwork required by different insurance companies makes it impossible to fully automate claims processing, resulting in thousands of lost hours filling out forms, raising costs and sometimes delaying care. In some cases, the costs of chasing payment for services exceeds the payment for those services. Yes, it sometimes makes more financial sense to just provide care without pay.
There are several layers to the billing cost problem, but they mostly relate back to an antiquated and defective fee-for-service payment model. That’s why my recent bipartisan primary care discussion draft establishes value-based payments at least for primary care, reducing reliance on fee-for-service payments, and eliminating billing and associated administrative costs altogether for certain services.
One particular scourge for patients is prior authorization: confusing, cumbersome, and inconsistent insurance rules that stop care while providers spend valuable time documenting and justifying the clinical need for a medicine or service. In a value-based system, where doctors make their money by reducing costs and keeping patients healthier, there’s no logic to prior authorization. I propose that companies in Medicare get prior authorization from CMS before they can impose prior authorization on doctors practicing in successful accountable care organizations (ACOs).
A 2022 Surgeon General Advisory report links administrative burdens with health care burnout, with less clinician time with patients, and even with harm to patients. The Surgeon General specifically called on insurers to “reduce requirements for prior authorizations, streamline paperwork requirements, and develop simplified, common billing forms.”
My reform legislation will require the Centers for Medicare and Medicaid Services first to identify the worst prior authorization practices in Medicare Advantage. Second it requires CMS to set common standards for common prior authorization requirements across insurance plans. Third, it will lift the prior authorization burden completely off providers in accountable care organizations with a proven track record of efficient patient care: no prior authorization without prior authorization. I doubt insurers will be able to justify prior authorization for value-based providers whose incentives align with theirs. Providers may have an incentive to run up their charges in a fee-for service model, but running up charges is self-defeating for ACOs.
In today’s hearing, we’ll discuss these and other solutions. We’ll hear from health economist David Cutler how administrative costs in the US are far higher than in other countries, and where savings can be found in the health care financial transaction ecosystem. We’ll hear from Rhode Island’s Noah Benedict, who leads one of our state’s highest-performing primary care practices, the Integra ACO, on how administrative burdens hurt his ACO patients.
As I have said many times during hearings of this committee, my focus is clear: let’s work on serious proposals that reduce health care spending with no – none, zero – benefit cuts. Such proposals are good for patients, good for doctors, and good for the budget.

As I turn to my ranking member, I’d like to thank Senator Grassley and his team for showing up at my health care savings “office hours” with several very helpful and promising ideas and suggestions. I look forward to working with you.
